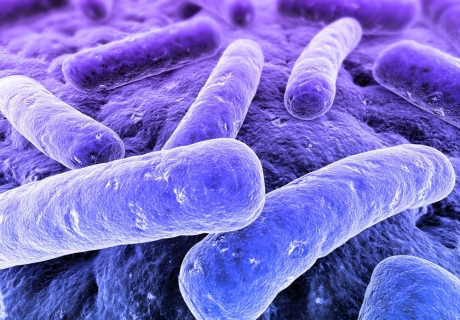
 Despite numerous campaigns and policies by the Government, bio-contamination continues to prevail in healthcare environments with a concerning 21,629 cases of E. coli reported since January 2012.
Despite numerous campaigns and policies by the Government, bio-contamination continues to prevail in healthcare environments with a concerning 21,629 cases of E. coli reported since January 2012.
Ian Hancox, CS’s coatings specialist, discusses how specialist finishes for interior walls and ceilings can help to reduce these figures and provide a safer and more hygienic hospital environment.
The alarming facts
The management and prevention of healthcare associated infections (HCAIs) is one of the biggest concerns for hospitals, with ‘superbugs’ such as Acinetobacter Baumannii & Clostridium Difficile continuing to affect both patients and healthcare staff. Approximately 300,000 patients develop a HCAI each year, which translates into an estimated 1 in 10 patients subjected to these fatal infections during their time at a UK hospital.
Commonly caused by the contaminated hands of healthcare workers and visitors, as well as contaminated medical devices and interior surfaces, and a failure of staff and visitors to comply with local policies, procedures and guidelines, the difficult to treat HCAIs complicate existing illnesses, causing stress to patients and their families and may even lead to death. Statistics show that patients who contracted a HCAI are around seven times more likely to die in hospital than unaffected patients, causing an estimated 5,000 patient deaths each year, which ultimately should have been avoided.
Together with the driving concern to protect patients, the safety and cost implications that the NHS incurs as a result of HCAIs, is putting huge pressure on health trusts to ensure that every step is taken to reduce the rate of infection, if not eliminate it. Costing an estimated £1 billion a year, hospitals have to manage the availability of beds, and with infected patients having to spend on average 11 extra days in hospital, those who acquire a HCAI whilst in hospital are costing the NHS three times more to treat and care for than those without a HCAI.
HCAI resistance
Reportedly in recent years, the healthcare industry has taken big steps to develop technological advancements to ensure the best protection for patients and the public. This includes innovations in stronger cleaning agents, improvements in cleaning policies, training and evolutions in hygiene prevention materials.
In particular, developments made in products used for interior wall and door finishes mean that hospitals can successfully reduce the prevalence of infections by specifying hygienic surfaces, employing specialist coatings or sheeting for walls and ceilings.
Providing protection against fungi and bacteria, including MRSA, Salmonella Typhimurium, Aspergillus Niger, E. coli 0157:H7 and many others, anti-microbial coatings are highly effective in infection control.
Formulated with a special high chemical resistance and containing non-leaching biocides, the seamless finish and smooth surface of these hygienic coatings make it difficult for bacteria to colonise and multiply.
Armed with added chemical & anti-microbial protection in each layer of the coating system, a quality coating should safeguard the interior environment against infection and impact for ten years, before requiring refurbishment. And due to the nature of the system, simple touch ups can easily be conducted with minimal impact on the area.
Most hygienic coatings are available in a variety of colours utilising BS 4800, RAL Classic or NCS 2nd series colour standards, as well as colour matching, enabling specifiers to create an environment conducive to recovery.
It is important that all coatings specified are compliant with legislation (VOC levels & Biocidal Product Directive or BPD) and the health building notes (HBN) such as HBN 26 ‘Facilities for surgical Procedures Vol.1’, and the Health Technical memorandums such as HTM 56 to ensure the best solutions for patients and medical staff throughout the building.
For areas which require additional durability against abrasion or impact from hospital beds and wheelchairs, specialist coatings are available with an additional fibreglass reinforcement option.
Selecting the right coating system
When specifying coating systems for all healthcare environments, it is important to consider the end use of the coating to ensure the correct level of chemical resistance is applied, taking into consideration the anticipated daily wear and tear and the substrate the coating is being applied to.
For instance, in non critical corridors and store rooms where less scrub resistance is required, a waterborne ‘super-emulsion’ system would be appropriate. With a very low odour and thick coating, it is ideal for busy areas used by both patients and staff and still protects against the spread of infection.
However where high volumes of stringent cleaning regimes are conducted – such as in theatres and post-op recovery areas – it is important to specify a very low odour, solvent free hygienic coating which ensures resistance against repeated cleaning with strong detergents and abrasives.
Strength of bacteria
According to the Health Protection Agency’s (HPA) Annual Report Accounts 2011/12, rates of HCAIs such as MRSA and Clostridium Difficile (CDiff) infections have dropped, based on last year’s figures.
Whilst this is, of course, a welcome result for healthcare facilities and hospitals nationwide, concern is growing as bacteria that destroy Carbapenem antibiotics (which are often the last line of effective treatment for patients with infections) is increasing.
These recent outbreaks in Carbapenem-resistant organisms, suggest that these multi-resistant bacteria are becoming established in the UK, in community and hospital settings. With this in mind, it is becoming more important for hospitals to ensure that infection is avoided from the outset and not given the chance to colonise and multiply. By using specialist anti-microbial coatings as an easy to apply, first step, supported by a stringent cleaning regime, bacteria will fail to inhabit.
Best practice
Everyone working in healthcare and healthcare research has a role to play in helping to prevent the spread of infection. So whilst medicines continue to develop to combat new strains of bacteria and viruses, internal healthcare environments must also evolve to provide clean and safe environments for all who visit.
Through good practice and careful hygiene control, it has been estimated that around 30% of HAIs can be avoided, so it is essential that we continue to stress the importance of such measures, on those who can help.
Sources: HAI Research Network and HPA (Health Protection Agency)

